-
-
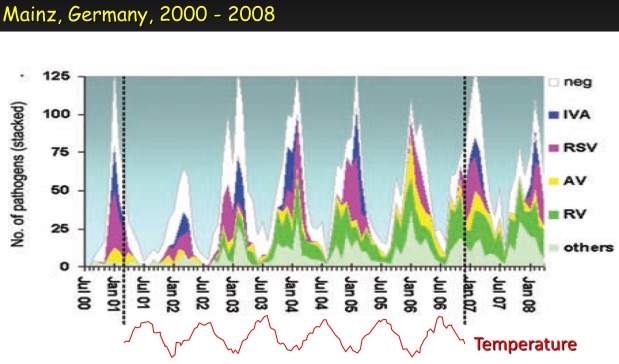
- Respiratory illness responds so quickly to changes in ambient temperature that conventional epidemiology can’t give a good description
- Data often show a “harvesting” mechanism, where temperature changes activate dormant colds and flu
- Colds and flu frequently appear in the rainy season in the Tropics
- Explanations based on increased transmission in cold, dry places can’t work in the Tropics!
-
Covid is a respiratory illness, although we don’t yet know how much it has in common with well-established (“seasonal”) respiratory illnesses. Modern epidemiological models clearly work very well for new illnesses at the point where they enter a population, and they work well for many other viral and bacterial outbreaks, but I’d like to suggest that they don’t work well for normal respiratory illnesses.
For example, we have the concepts of (i) the average number of previously unexposed individuals infected by a single, freshly introduced disease carrier (R0), and (ii) the average number of secondary infections caused by an infectious individual at a given point in the outbreak’s progression (R). But would either these parameters have been very helpful for understanding colds and flu in the winter of 1925 – 26 in the Netherlands?

The black solid and dotted lines show the numbers of colds and flu cases in seven regions of the country in that winter, while the colored lines show inverted outdoor temperatures (ie low temps at the top and high temps at the bottom) for five Dutch weather stations during the same period. Clearly, any model that doesn’t take temperature into account is not going to be much use. For one thing, during the first half of the cold season, there is an extraordinary degree of synchronization between the different regions, with no evidence of waves of infection moving around the country. This suggests a “harvesting” mechanism, where the infection moves in advance, but observable illness is triggered by temperature changes. I’ve pasted several other examples below.
It seems that low temperature and low humidity slightly favored the spread of CoV-2 in Chinese cities in January 2020 [1]. This makes it like influenza, which is another virus that has a lipid envelope. However, it’s the effect of temperature that seems to be most important. For example, rhinovirus (which is normally mild but can cause the deaths of children and old people) has no lipid envelope, and survives longest in humid conditions, but, like influenza, it is most common in winter. Influenza is obviously favoured by cold temperatures but it’s also common in hot, humid places. For example, it appears every year in the Brazilian city of Fortaleza (which is close to the equator) during the rainy season. In fact A/H3N2 influenza circulates continuously in East and Southeast Asia, and spreads to temperate regions from this network [2]. All strains of influenza also spread from colder to warmer countries, although at a slower rate. This shows that influenza can adapt its activity to different climates quite rapidly. For example, the same study showed that 50% of European A/H3N2 influenza strains were descended from strains that were in tropical or subtropical regions one year earlier [2]. We don’t yet know how Covid will respond to the warmer weather of spring and summer, but it’s a fair guess that it will eventually become like almost every other respiratory virus, with clear winter seasonality.
Please see the other pages of this blog for my thoughts, especially the following pages:
https://oldwivesandvirologists.blog/predicting-the-seasonality-of-covid/
https://oldwivesandvirologists.blog/
[1] Wang, Jingyuan, et al. “High Temperature and High Humidity Reduce the Transmission of COVID-19.” https://papers.ssrn.com/sol3/Papers.cfm?abstract_id=3551767
[2] Bedford, Trevor, et al. “Global circulation patterns of seasonal influenza viruses vary with antigenic drift.” Nature 523.7559 (2015): 217-220.
_______________________________

The viruses that caused respiratory tract infections in hospitalized children in Buenos Aires, Argentina, which has humid subtropical climate, 1998 – 2003. The four most frequent pathogens were, in order, respiratory syncytial virus, influenza A, adenovirus, and parainfluenza. From Viegas M et al. J Infection 2004; 49(3):222–8.

The Hypothesis
For a general discussion of the seasonality of respiratory viruses, written for the layperson, please see
Every winter, colds and flu increase
For detailed scientific information about the seasonality of respiratory viruses, including discussion of the trade-off model, viral dormancy and much else, see my 2016 paper:
Also:
For a discussion of the strange timing and duration of influenza epidemics, please see
The strange arrivals – and departures – of influenza epidemics in the UK, 1946-1974
Applications to Covid-19
For information about the probable seasonality of Covid-19, and whether we can expect it to become rarer in the summer, or reappear in the fall, please see
Predicting the seasonality of Covid-19
For discussion of how the trade-off model can be applied to the Covid epidemic see
Covid 19 and the trade-off model
For a simple model of the transmission of viruses such as CoV-2, please see
A simple model of CoV-2 transmission
For comments about how quickly we can expect viruses to adapt to new environments, please see
Adaptability or respiratory viruses
For more detailed scientific points about CoV-2, see
Technical notes on CoV-2 for scientists
For practical tips on avoiding respiratory illness see
Suggestions for avoiding colds and flu – and Covid-19


One thought on “Epidemiology of respiratory illness”