. . . . and poor clothing, cold weather, wind and rain all increase respiratory illness. How can we explain this?
(also on Spotify)
By Patrick Shaw Stewart, March 2017
It’s late March, and I’m traveling through northern India as I write this. At this time of year the temperature rises above 37°C every day, so you might be surprised to hear that a high proportion of the population has a cold at the moment. On buses, in airports and on planes, you hear someone coughing or sneezing every few seconds, and most of the taxi drivers who have given me a ride were sniffing, coughing and spitting. (It’ll be a miracle if I get home without suffering in the same way!) I saw something similar the first time I came to India a few years ago, and it started me thinking about respiratory viruses, because I could see that the conventional explanations of the seasonality of colds and flu just weren’t going to work here in India.
In fact I travel for work in many different countries, and I’ve taken to asking the people I meet (scientists, mainly) whether the general population in their country believes that cold weather and chilling will increase the chance of getting a cold. The response has been a very clear “yes”. Whether or not my friends believe it themselves, they all agree that the man or woman in the street believes it. This belief seems to be universally present throughout the world, although it takes different forms. A famous English folk-song says that venturing on to Ilkley Moor without a hat will be fatal. In 1902 Beatrix Potter wrote The Tale of Peter Rabbit, who caught a cold after he hid from the gardener Mr. McGregor in a watering-can. In Russia parents worry – much more than we do in the UK – when, for example, their children leave a swimming pool with wet hair. In Tokyo, cold clear weather is thought to cause the trouble. In South China, Singapore and Indonesia wind and rain are the culprits, while in Fortaleza (northern Brazil) it’s clear to everyone that colds and flu make their appearance in the rainy season. Here in India, some people say that cold epidemics are caused by the daily 12°C fluctuations, while others think it’s got something to do with air conditioning.
Most doctors and scientists were taught at university – as I was – that this is all an “old wives’ tale”. We were told that chilling of the human host has absolutely no effect on coughs and colds. This has caused a lot of trouble, because we all know that colds and flu are seasonal; they are roughly 50 times more common in temperate regions in mid-winter than high summer, and we need an explanation. Moreover, modern record-keeping makes it very clear that cold snaps are usually followed by increased sickness and more deaths from respiratory disease. It’s also very surprising that almost every common viral respiratory pathogen is affected in the same way – with cold weather and rain increasing sickness (see the references at the end of this essay, especially the papers by Du Prel, Viegas and Chew). This is, I believe, one of the great unsolved mysteries of medical biology. Whether one looks at DNA viruses, positive-sense RNA viruses, negative-sense RNA viruses, lipid encapsulated, non-encapsulated, icosahedral, filamentous viruses etc., roughly the same patterns appear. (In fact, the only exception I know of is that in 1981 Edgar Hope-Simpson found that parainfluenza type 3 was slightly more common in the warmer six months than in the colder** .)

Some characteristics of human respiratory viruses.
As a result, a cottage industry of scientific publication has sprung up, with scientists all over the world reporting on the influence of weather etc. in their city or region, usually with an acknowledgment that there is no good scientific explanation of their findings. Instead of going back to first principles and trying to come up with explanations that do work, science seems to have put the whole problem into the “too difficult” box, and is busy ignoring it. There have been attempts at rational explanation, discussed below, but all the well-known ideas are either incompatible with tropical observations, or apply only to certain strains. For example, a fashionable explanation of influenza seasonality could work for that virus, but it would give the opposite prediction for rhinovirus – although both viruses are (of course) much more common in winter. We should be looking instead for an explanation or explanations that can explain the seasonality of all – or almost all – common respiratory viruses.
The unhelpful training that I and others received at university seems to be the result of the misinterpretation of a series of experiments in the 1950s and 60s, described below, where volunteers were chilled after being inoculated with a respiratory virus. They might have been good experiments, but the conclusions drawn are simply wrong – a realization that is becoming increasingly obvious.
In a moment I will give you what I think is the correct explanation, but first some natural history is needed. Viruses are quite often seen to jump from one species to another, and it’s obvious that this has been going on for millennia. (Here we can think about all classes of animal viruses, not just respiratory ones.) Strangely – and this is a key observation – viruses that switch rides are at first often more dangerous than strains that have persisted for several centuries in the same host species. The various “haemorrhagic fevers” that humans catch from other animals (including mice and ticks), Ebola, SARS, HIV and bird flu are all examples. Myxomatosis, an insect-borne virus that spread from wild rabbits in South America to European rabbits, is another. Such viruses are unusually dangerous, and quite often cause the death of their host. This implies that over time an equilibrium is reached as a virus adapts to its host, with the most successful strains developing intermediate levels of virulence – not too passive, but not too aggressive either. This makes logical sense. A virus that has a long incubation period and doesn’t at first give its human or animal host a high fever is likely to spread further and faster than one that very aggressively attacks its host, such as Ebola virus. In other words it’s probably not a coincidence that viral diseases are often inconvenient, but seldom fatal, and that they don’t actually make complex multicellular animals impossible. This moderating selection probably acts especially strongly in prosperous modern human societies, because we have the luxury of staying at home and going to bed when we feel unwell or have a fever. But note that other animals show similar behavior: a cow with foot-and-mouth disease doesn’t usually move around and mix with other cows – it will generally stand in a corner of a field, and be very reluctant to move – even when shoved by a farmer or vet.
The idea that this kind of equilibrium will be established isn’t new. It’s predicted by the “trade-off” model of virulence. This model suggests that the benefits of virulence (in particular the increased rate of virus production and shedding) are balanced against the reduction of the time during which shedding takes place, and also by changes in the behavior of hosts, when virulence is too great.
How does this relate to seasonality? Well, it gives us the crucial insight that (as a result of medium-term evolution) viruses generally moderate their virulence. They also need to control which parts of the body they infect – for example, infecting the heart or the nervous system is a bad idea, because both are likely to stop your host from moving around, or worse, to kill it. Since almost all respiratory viruses are much more common in winter than in summer, we have a clue: the key to understanding viral responses may lie in temperature-sensitivity.
Viruses are very simple – and they have very limited options for adapting their behavior to different situations. If they find themselves next to a solid surface they can either stick to it, or float away. If they are inside a cell they can either remain dormant, or they can try to replicate themselves. The respiratory tract happens to be one of the coldest parts of the body. The subsegmental bronchi usually have a temperature of around 35°C, but the glottis tends to be around 24°C. In fact there’s a temperature gradient from the nose to the lungs, with the temperature near the nose and throat varying when the seasons change, when weather events impact ambient temperature, and when the host takes exercise or gets wet (chilling rapidly reduces the blood supply to the respiratory tract). One smart way (from the virus’s point of view) to avoid infecting the lungs and gut is therefore to make use of temperature – one of the few parameters that a virus can keep tabs on. So, imagine this: a virion (virus particle) that is bumping up against the surface of a cell on the lining the lungs at 35°C, chooses not to stick. (The “choice” here is an evolutionary choice – a result of natural selection.) A little later it is “escalated” up the respiratory tract (by what is called the mucocilary escalator – the complex system of ciliated and mucous-secreting cells that keeps our lungs clear) and it finds itself in a similar situation at 24°C, near the glottis. Now, it sticks – and it’s in a good place to cause an infection that might spread to other hosts. It might enter the cell and start to replicate, or it might sit tight for a while. Viruses can benefit from acting in unison, so it might be helpful to remain dormant for the time being (inside or outside the cell – scientific investigation will be needed to find the exact location or locations). Later on, if the temperature drops to say 22°C, it might become active – again sensing temperature – and hundreds or thousands of other virions might become active at the same time, all triggered by a temperature fluctuation near the glottis. (Note that Antarctic and recent PCR studies have both shown the reality of viral dormancy and reactivation – see the references below.)
My suggestion is that the seasonality of viruses and the appearance of viral epidemics after cold snaps are both side-effects of the natural biochemical temperature-sensitivity of virtually all respiratory viruses. This property can allow viruses to cause severe local infections without incapacitating the host – and obviously the resulting irritation can cause coughing, sneezing and runny noses, all of which will help to transmit the virus.
I wrote a paper about viral temperature-sensitivity and seasonality recently, where I labelled this mechanism “M4” [ref.1].
Now there are several other explanations of seasonality that are popular with scientists (categorized as M1, M2 and M3 in my paper), but it’s generally acknowledged in the scientific literature that none of them can do a good job of explaining the behavior of viruses. For example, some scientists have suggested that we tend to stay indoors and crowd together more in winter than in summer, which increases transmission (M1). Others point out that some virus particles suspended in air can survive longer in cold, dry, wintery conditions (M2). A third explanation is based on the idea that our immune defenses are somehow weaker in winter (which, studies of vaccination have shown, in general they’re not! M3). However, there is one very fundamental objection that rules out all these mechanisms as the principal drivers of seasonality: although the same or very similar viruses cause infections all over the world, viral respiratory diseases are more common in the tropics year-round than in the summer in temperate zones. (For examples, click on the Figures on the right-hand Sidebar, or below if you are looking at this on mobile phone.) This is hard to explain! Whichever of these alternative explanations (M1 – M3) you focus on, the parameters are more extreme in the tropics than in temperate summers. There may be less sunshine, less moisture in the air, and we may stay indoors more in the winter than in the summer (in temperate regions), but isn’t there even more sunshine, more moisture in the air, and don’t people – at least poor people – stay outdoors even more in the tropics than in the summer where I live?
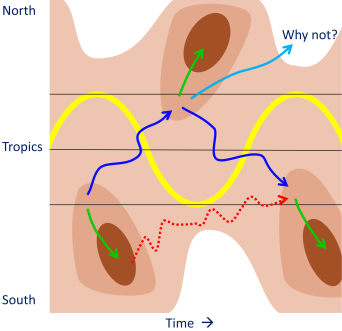
The strange global distribution and seasonality of influenza and other viral respiratory illnesses, shown schematically. Time is indicated across the figure, while latitude is indicated from top to bottom. Levels of respiratory illness are indicated by brown shading, with dark brown showing the highest rates of infection. The yellow curve shows the path of vertical solar radiation. The strange distribution of respiratory illness is shown, with more illness in the tropics throughout the year than in temperate regions during the summer months. In particular, we need to explain why viruses that have travelled in the direction indicated by the pale blue arrow do not thrive in temperate regions during the summer months.
There are other problems with M1 – M3 as explanations of seasonality. Epidemics often arrive throughout wide geographical areas in an extraordinarily well-synchronized way. Johannes van Loghem, a Dutch professor of Hygiene, was one of the first to observe this in the 1920s [ref.2, and click on the first Figure on the right-hand Sidebar – below on a mobile phone]. He found that – roughly one week after ambient temperature dropped – cold epidemics arrived almost simultaneously throughout the whole of the Netherlands. There was no evidence of waves of infection moving around the country, which would be predicted by mechanisms M1 – M3. Edgar Hope-Simpson saw something very similar when he compared influenza in Prague (Czechoslovakia) with the same illness in his medical practice in Cirencester, UK, where he carefully identified the flu strains involved (see the second Figure on the right-hand Sidebar or below). Spikes of influenza appeared almost simultaneously in the two locations, in spite of antigenic shifts from Hong Kong to English flu in 1972, and from influenza A to influenza B in 1973 [ref. 3]. Again, there were no signs of waves of infection that moved across Europe.
The last explanation (M3), the suggestion that our immune systems are weaker in winter than summer, is also incompatible with the experiments that caused so much of the trouble in the first place. As I mentioned before, in the 1950s and 60s hundreds of volunteers were first kept in quarantine, then inoculated with an (unidentified) recycled “pedigree” virus (which was passed from volunteers to subsequent batches of volunteers in later experiments). Some individuals were then chilled, while others stayed warm. No significant difference between the two groups in the number of colds was seen, and the researchers concluded that chilling did not bring on colds. This was repeated over many years and in different laboratories. Now, if our immune systems are weaker after chilling, why didn’t these experiments give increased infection rates after chilling?
My simple suggestion (M4) that almost all cold viruses are temperature-sensitive can, I believe, solve all these problems:
- M4 predicts that respiratory illness will be more common in the winter because, as the temperature drops, viruses that are present in our respiratory tracts will become more active. In spring, when the temperature rises, they will become less active. In the case of rhinovirus, it was recently shown that the virus then remained dormant (or hidden, anyway) over the summer [ref. 4].
- M4 also suggests that viruses can adapt to life (if viruses can be considered to be alive) in tropical locations. As I mentioned earlier, there’s a temperature gradient in the respiratory tract (RT) from the nose to the lungs. Therefore, in warmer climates we might anticipate that respiratory viruses would colonize the RT closer to the nose, while in cold climates the same strain would naturally colonize the RT closer to the lungs. It should also be possible for viruses to rapidly lose or gain temperature-sensitivity as they move or are transported around the world – they have very high mutation rates and can evolve very quickly. When a strain arrives in a new location, it will therefore be able to adjust its temperature-sensitivity reasonably quickly to the local climate – which it needs to to in order to transmit itself efficiently.
I must also comment from personal experience that it’s noticeable that if you pick up a cold in the tropics and return to the UK it often goes to the lungs and tends to be particularly nasty and unusually persistent! Note that studies show that influenza moves from hot climates to cold ones more frequently than it moves in the opposite direction [ref.5, check out Extended Data Figure 3].
- According to M4, the reason for the failure of the classic 1950s and 60s experiments to show an effect of chilling was most likely the investigators’ choice of viral strains. They generally used ‘‘pedigree” strains that were passed from volunteers to subsequent batches of volunteers in later experiments. These pedigree strains may have lost part of their temperature-sensitivity (particularly with regard to the early steps of infection, binding and cell entry) because the investigators may have accidentally or deliberately selected strains that gave colds quickly.
(Please note that I’m not saying that M1 – M2 have no effect on respiratory illness. Clearly if we e.g. crowd together in a pub or school this can help to spread colds and flu. I’m just saying that they’re not the main drivers of seasonality.)
Why is this important? I was taught at school that science is about understanding the world around us. There is often a debate about whether it’s better to carry out fundamental research or to work on more practical applied subjects. The answer that is often given is that you can never predict the practical benefits of fundamental research, so we should try to get the fundamental understanding in place first. A rational approach would start with the key questions of the response of respiratory viruses to host chilling, and viral seasonality, which early 20th century scientists grappled with before they even knew what a virus was [ref.2].
It’s also extraordinary that some obvious avenues for practical research have been neglected by doctors and microbiologists – apparently because they conflict with established dogma. Twenty years ago a consortium of European scientists set out to apply the techniques of market research to discover whether different climates, and different steps taken to protect against cold, influenced winter mortality in eight European regions, ranging from northern Finland to Athens [ref.6]. They showed that standing still outside for more than two minutes (p=0.04), wearing a skirt (p=0.005), and shivering outside (p=0.001) are all dangerous activities because they increase the probability of dying from respiratory disease (see the sixth Figure on the right-hand Sidebar, or below on mobile phones). On the other hand, wearing an anorak (p=<0.001) and taking outdoor exercise sufficient to cause sweating (p=0.02) are strongly protective. This publication is regularly cited by papers that show for the umpteenth time that respiratory illness increases when ambient temperature drops (in some particular part of the world), but no-one has taken the obvious step of following up the practical implications of this paper. For example no-one has investigated whether old people can be protected by going outside in cold weather, well wrapped-up, to take brisk exercise. It seems that the experts won’t try this kind of thing because they “know” it won’t work.
What is needed is empirical evidence. These problems could be tackled at many levels. For example, (i) experiments could be carried out with volunteers, with some participants being chilled and others not – this time relying on “wild” viruses that the volunteers happen to be carrying (rather than inoculating them with massive doses of artificial “pedigree” or laboratory strains). (ii) Animal experiments with wild and “labelled” viruses could be carried out to investigate both the transmission and localization of virions in the respiratory tract. (iii) The temperature-sensitivity of the various steps of cell entry and replication in both wild and laboratory viruses could be investigated in cell-cultures – much of the data that is available now was collected by accident in studies that were designed to investigate something else. (iv) The DNA and RNA sequences of wild and laboratory viruses could be analyzed, focusing particularly on something called “RNA secondary structure” that a lot of my readers will know about. (v) Epidemiologists and bioinformaticians could investigate changes in sequences and virulence in a variety of viral species as they move around the world. Hundreds of thousands of people – sometimes millions – die every year of respiratory illness, particularly the very old and the very young. All these experiments have the potential to answer fundamental questions, provide practical solutions, and save lives.
I’ve put these points to several well-known virologists in the UK and abroad. I’ve also given a talk at an international virology meeting (and I thank the organizers for giving me the opportunity), where I was able to show my scientific poster to many microbiologists. I have found it very difficult to get scientists to focus on the fundamental issues, and the majority won’t read my paper and don’t engage with the arguments. In fact they sometimes ignore the clearly-stated conclusions of their own papers!
Which is all very surprising.
Patrick Shaw Stewart, March 2017
Papers directly mentioned above:
[2] Van Loghem JJ. An epidemiological contribution to the knowledge of the respiratory diseases. J Hyg 1928; 28(01):33–54.
[3] Hope-Simpson, R. E. (1981). Parainfluenza virus infections in the Cirencester survey: seasonal and other characteristics. Epidemiology & Infection, 87(3), 393-406.
[4] Granados A, Goodall EC, Luinstra K, Smieja M, Mahony J. Comparison of asymptomatic and symptomatic rhinovirus infections in university students: incidence, species diversity, and viral load. Diagn Microbiol Infect Dis 2015; 82 (4):292–6.
[5] Bedford, T., Riley, S., Barr, I.G., Broor, S., Chadha, M., Cox, N.J., Daniels, R.S., Gunasekaran, C.P., Hurt, A.C., Kelso, A. and Klimov, A., 2015. Global circulation patterns of seasonal influenza viruses vary with antigenic drift. Nature, 523(7559), p.217.
[6] Donaldson G. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The Eurowinter Group. Lancet 1997; 349:1341–6.
[7] **I was very interested to see that a 2018 study in Edinburgh found exactly the same thing. To quote the authors, “HPIV-3 (human parainfluenza virus, type 3) is the only virus to prefer above average temperatures (9.4 °C)”. The study tracked 9 common respiratory viruses. Reference: Price, R. H. M., Graham, C., & Ramalingam, S. (2019). Association between viral seasonality and meteorological factors. Scientific reports, 9(1), 1-11.
Other key references:
Mudd S, Grant SB. Reactions to chilling of the body surface: experimental study of a possible mechanism for the excitation of infections of the pharynx and tonsils. J Med Res 1919; 40(1):53.
Andrewes CH. Adventures among viruses. III. The puzzle of the common cold. N Engl J Med 1950; 242(7):235–40.
Dowling HF, Jackson GG, Spiesman IG, Inouye T. Transmission of the common cold to volunteers under controlled conditions III. The effect of chilling of the subjects upon susceptibility. Am J Epidemiol 1958; 68(1):59–65.
Allen TR, Bradburne AF, Stott EJ, Goodwin CS, Tyrrell DAJ. An outbreak of common colds at an Antarctic base after seventeen weeks of complete isolation. J Hyg 1973; 71(04):657–67.
Muchmore HG, Parkinson AJ, Humphries JE, Scott EN, McIntosh DA, Scott LV, et al. Persistent parainfluenza virus shedding during isolation at the South Pole. Nature 1981; 289:187–9.
Morikawa S, Hiroi S, Kase T. Detection of respiratory viruses in gargle specimens of healthy children. J Clin Virol 2015.
Randall RE, Griffin DE. Within host RNA virus persistence: mechanisms and consequences. Current Opinion in Virology 2017, 23:35–42.
Du Prel JB, Puppe W, Gröndahl B, Knuf M, Weigl F, Schaaff F, et al. Are meteorological parameters associated with acute respiratory tract infections? Clin Infect Dis 2009; 49(6):861–8.
Viegas M, Barrero PR, Maffey AF, Mistchenko AS. Respiratory viruses seasonality in children under five years of age in Buenos Aires, Argentina. A five-year analysis. J Infection 2004; 49(3):222–8.
Chew FT, Doraisingham S, Ling AE, Kumarasinghe G, Lee BW. Seasonal trends of viral respiratory tract infections in the tropics. Epidemiol Infect 1998; 121 (01):121–8.
Russell PH. Newcastle disease virus and two influenza viruses: differing effects of acid and temperature on the uptake of infectious virus into bovine and canine kidney cell lines. Arch Virol 1986; 88(3–4):159–66.
Kashiwagi T, Hara K, Nakazono Y, Hamada N, Watanabe H. Artificial hybrids of influenza A virus RNA polymerase reveal PA subunit modulates its thermal sensitivity. PLoS ONE 2010; 5(12):e15140.
Dalton RM, Mullin AE, Amorim MJ, Medcalf E, Tiley LS, Digard P. Temperature sensitive influenza A virus genome replication results from low thermal stability of polymerase-cRNA complexes. Virol J 2006; 3:58.
Applications to Covid-19
For information about the probable seasonality of Covid-19, and whether we can expect it to become rarer in the summer, or reappear in the fall, please see
Predicting the seasonality of Covid-19
For comments about the epidemiology of Covid and other respiratory illnesses, please see
Epidemiology of respiratory illness
For discussion of how the trade-off model can be applied to the Covid epidemic see
Covid 19 and the trade-off model
For a simple model of the transmission of viruses such as CoV-2, please see
A simple model of CoV-2 transmission
For comments about how quickly we can expect viruses to adapt to new environments, please see
Adaptability or respiratory viruses
For more detailed scientific points about CoV-2, see
Technical notes on CoV-2 for scientists
For practical tips on avoiding respiratory illness see
Suggestions for avoiding colds and flu – and Covid-19
Also
Your brief survey of old wives tales from around the world reminds me of my experience in China’s Northeast, where winter temperatures could drop to -30C. My lack of respect for the cold and, particularly, for the change of season, earned me a sharp rebuke on more than one occasion. Local belief, among ‘old wives’, in the traditional agricultural calendar was pretty strong, and I was often informed that the calendar predicted the coming days were going to bring certain conditions, ‘So watch out. Wrap up well!’. It may be confirmation bias, but they did seem frequently correct.
The locals were not at all interested in showing how hardy they were, and people would wear three pairs of trousers (including knitted long johns) from ridiculously early in the autunm, until well past the point I was back in shirt sleeves (at least during my first few of years there). This fitted with exhortations to pay particular attention when the temperature was changing – those points in autumn when the temperature takes a sudden dip, and in spring when there may be a sudden rise, or a ‘false start’ before temperatures turned down again.
Could change in temperature, rather than absolute temperature, play a part?
LikeLike
It’s all ABOUT change in temperature.
I’m not sure about upwards changes in temperature. They have a similar tradition in India. They say if the temperature rises too fast you can get sick – the cure is bathing in cold water. I can imagine that if the temperature rose fast certain bound viruses could be released, and could cause trouble somewhere else in the resp tract – especially if they moved towards the (colder) nose.
LikeLike
Right. Time I got back to that video to understand this properly before commenting further!
LikeLike